
Lip filler necrosis is one of the most feared complications in aesthetic medicine but it’s also highly preventable with proper training, technique, and rapid intervention. For aesthetic practitioners, recognizing the early warning signs and knowing how to act swiftly can be the difference between a full recovery and long-term damage.
What Is Lip Filler Necrosis and How Does It Occur?
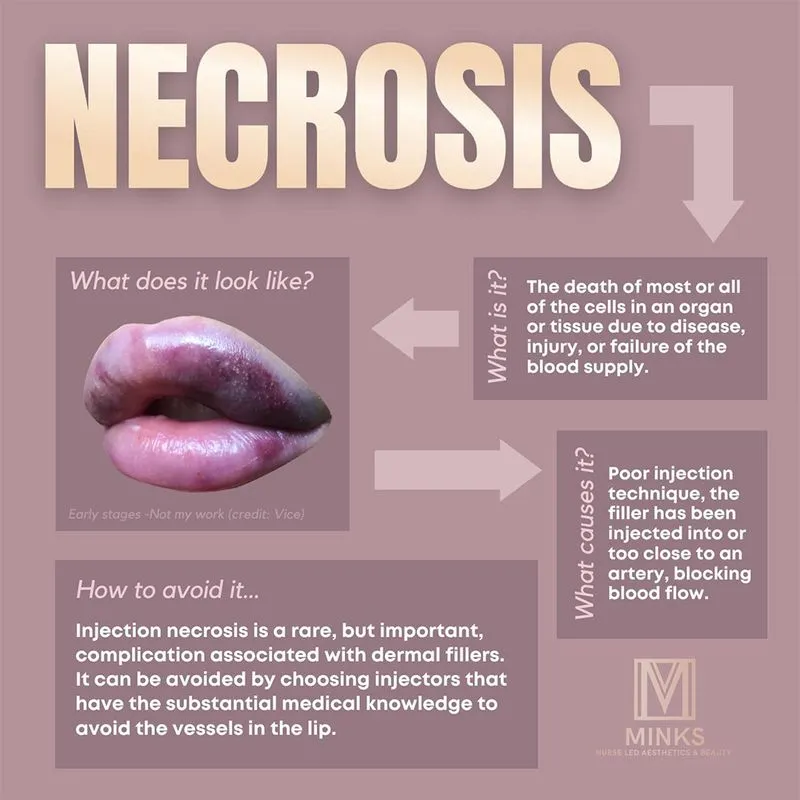
Lip filler necrosis is the death of lip tissue due to compromised blood supply, typically caused by vascular occlusion during dermal filler injections. It occurs when a filler is accidentally injected into an artery or compresses nearby vessels, reducing or entirely blocking blood flow to the tissue.
Without sufficient blood supply, the tissue becomes ischemic and eventually necrotic if not treated promptly. Though rare, necrosis from lip filler is a medical emergency. The lip area is especially vulnerable due to its rich vascular network and thin skin, making precision and anatomical knowledge essential during injections.

Early Warning Signs and Symptoms of Lip Filler Necrosis
Recognizing the first signs of necrosis after lip filler is essential for timely intervention and minimizing long-term tissue damage. While some symptoms can appear immediately during the procedure, others may be delayed, emerging hours after the injection.
The most common and telling symptom is pain, especially when it is severe, persistent, or disproportionate to what is typically expected after filler treatment. Unlike normal post-procedural discomfort, this pain often intensifies rather than subsides over time. Another key indicator is blanching, or the appearance of pale or white areas on the lips, which suggests restricted blood flow.
This may be accompanied by delayed capillary refill time when pressing and releasing the skin, a sign that the tissue is not receiving adequate perfusion. Discoloration progressing to a mottled or dusky appearance is also a red flag, as is a noticeable coolness in the area upon touch. Swelling may occur alongside these symptoms, particularly if it is localized, firm, and accompanied by tenderness.
In more advanced stages, lip filler necrosis symptoms can evolve to include the development of darkened patches, ulceration, and tissue breakdown. Prompt recognition of these warning signs, by both patients and practitioners is critical, as early treatment offers the best chance of full recovery without scarring or permanent damage.

Common Causes of Lip Filler Necrosis
Several factors can contribute to necrosis after lip filler, the most common being vascular occlusion, as mentioned before. One major risk is intravascular injection when the needle penetrates a vessel and filler is directly introduced into the lumen. This risk is heightened when injectors lack comprehensive anatomical knowledge or underestimate the complexity of vascular networks in the lips and perioral area. High-pressure injections can also increase the likelihood of vessel compression or rupture.
Poor technique, such as injecting too quickly, too deeply, or in large boluses, can significantly raise the risk of tissue ischemia. Repetitive treatments in the same area may create scar tissue or vascular fragility, further elevating the risk. Additionally, using large volumes of filler in delicate regions without the appropriate technique can overwhelm the tissue and obstruct blood supply.
Altogether, these factors underline the importance of precise technique, product selection tailored to the patient’s anatomy. As well as ongoing education, such as enrolling into an aesthetics complications course to maintain safety in lip augmentation procedures.

Prevention Techniques for Avoiding Vascular Occlusion and Necrosis
The best way to treat necrosis is to prevent it. Preventative strategies include a combination of advanced anatomical understanding and meticulous technique, often covered in specialized Lip Augmentation Training.
Effective prevention techniques include:
- Aspiration before injecting (though not foolproof).
- Using small volumes per injection site.
- Injecting slowly and with minimal pressure.
- Using cannulas in high-risk areas when appropriate.
- Continually moving the needle to avoid bolus injections.
- Avoiding overly superficial or deep injections.
Emergency Response Steps for Filler-Related Necrosis
If necrosis after lip filler is suspected, time is of the essence. Every injector should follow a pre-established emergency protocol, ideally taught in a lip filler training program.
Immediate steps include:
- Stop injecting immediately.
- Assess capillary refill time and discoloration.
- Massage the area gently to promote circulation.
- Apply warm compresses to support vasodilation.
- Administer high-dose hyaluronidase to dissolve the filler.
- Repeat hyaluronidase as needed per protocol.
- Refer to emergency care if no improvement occurs.
Early action can fully reverse the damage in many cases. Delayed necrosis after lip filler may require more aggressive intervention, including antibiotics or wound care.
Injector Protocols for Risk Reduction and Patient Education
Preventing lip filler necrosis requires more than excellent technique, it demands a comprehensive, protocol-driven approach that covers every stage of patient care. Skilled aesthetic injectors don’t just react to complications - they actively work to prevent them through thorough planning, continuous education, and clear communication with patients.
Here are the essential best practices in protocol and education:
- Pre-treatment consultations covering potential risks: A thorough consultation before treatment allows the injector to assess patient suitability, medical history, and potential contraindications. This is also when you explain the rare but serious risks, such as vascular occlusion and necrosis, in a calm, informative manner. Setting expectations ensures the patient is not caught off guard and understands the importance of post-treatment vigilance.
- Written consent that includes possible vascular complications: Informed consent is a legal and ethical necessity. It should specifically outline the risks of vascular occlusion, lip necrosis, and the signs to watch for post-procedure. Consent forms should be easy to understand and allow patients to ask questions. This documentation also protects the practitioner should any complications arise.
- Thorough documentation of the procedure: Accurate record-keeping includes the product used (brand, batch number), injection sites, technique, volume injected, and whether aspiration was performed. This detailed documentation supports continuity of care and is essential if the patient requires emergency intervention or reports post-treatment issues.
- Training staff to identify red flags: Every team member, from medical assistants to front desk staff, should be trained to recognize early signs of lip filler necrosis symptoms. For example, if a patient calls reporting severe pain, color changes, or numbness, staff should be instructed to escalate the concern to a medical professional immediately.
- Providing detailed aftercare instructions: Patients should leave with both verbal and written aftercare instructions that clearly explain what is normal (e.g., mild swelling, slight bruising) versus what is not (e.g., blanching, persistent pain, skin discoloration). Emphasizing the importance of reporting symptoms early can reduce the risk of delayed necrosis from lip filler going unnoticed.
- Following up with patients post-treatment: Post-procedure follow-up (via phone, message, or in-person) reinforces safety and builds trust. A 24 to 48-hour check-in is ideal, especially for new patients or high-risk areas like the lips.

Difference Between Vascular Occlusion and Lip Filler Necrosis
Although often discussed together, vascular occlusion and lip filler necrosis are not the same. Vascular occlusion lip filler refers to the blockage itself, while necrosis is the tissue death that results from prolonged occlusion.
Sometimes patients confuse lip filler bruising vs necrosis. Bruising is common and harmless, whereas necrosis involves progressive pain, blanching, and possible ulceration. The ability to distinguish whether it’s bruise or vascular occlusion is critical since being able to differentiate them may prevent the onset of necrosis.
Can Filler Necrosis Be Reversed?
When caught early, necrosis from lip filler can often be reversed without permanent damage. Hyaluronidase remains the gold standard in treatment, breaking down hyaluronic acid-based fillers and restoring blood flow.
Reversal is most effective within the first few hours after symptom onset. Once tissue necrosis sets in, healing may require weeks and involve additional medical support such as debridement, antibiotics, or referral to dermatology or plastic surgery. Patients who’ve seen pictures of lip necrosis after filler often fear the worst, but these severe outcomes are typically the result of mismanagement or delayed treatment.
The Bottom Line
Lip filler necrosis is a rare but serious complication that underscores the importance of expertise in aesthetic medicine. For injectors, mastering anatomy, recognizing early signs, and acting quickly can mean the difference between a minor issue and a lasting injury. Patients undergoing lip filler procedures deserve clear, confident communication that highlights both the risks and the safeguards in place to protect them.
References:
- Bruna Souza Felix Bravo, et al. Delayed-type Necrosis after Soft-tissue Augmentation with Hyaluronic Acid. PMC. JCAD. 2015. https://pmc.ncbi.nlm.nih.gov/articles/PMC4689510/
- Wang, R.; et al. Hyaluronic acid filler-induced vascular occlusion- Three case reports and overview of prevention and treatment. PubMed. 2023. https://pubmed.ncbi.nlm.nih.gov/38131127/
- Cuma Çakmak and Özgür Uğurluoğlu. The Effects of Patient-Centered Communication on Patient Engagement, Health-Related Quality of Life, Service Quality Perception and Patient Satisfaction in Patients with Cancer: A Cross-Sectional Study in Türkiye. PMC. 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC10901059/
Disclaimer:
This article is intended for licensed medical professionals. All protocols, dosages, and treatment insights referenced herein are based on published literature. The content is not intended to encourage application, diagnosis, or self-treatment of unlicensed individuals, and should not be used as a substitute for the clinical judgment of a qualified healthcare provider.

