
When performing aesthetic procedures such as dermal filler injections, understanding the difference between a simple bruise and a vascular occlusion is not just helpful - it’s critical. While bruising is a common, usually harmless side effect, vascular occlusion is a rare but serious medical emergency that requires prompt recognition and intervention.
Failing to distinguish between these two can lead to devastating outcomes, including tissue necrosis or even blindness. This guide will walk you through everything medical aestheticians need to know to spot the signs, act quickly, and prioritize patient safety.
Importance of Differentiating Between Bruising and Vascular Occlusion
Distinguishing between bruising and vascular occlusion is essential to prevent severe complications. A bruise may look alarming to a patient, but it’s typically benign. In contrast, a vascular occlusion is an interruption in blood flow due to a filler blocking a vessel, and it can cause irreversible damage if not addressed within hours.
Clinicians must assess symptoms quickly and accurately. Bruising presents with skin discoloration but is rarely accompanied by significant pain or other symptoms. Vascular occlusion may appear subtle initially but progresses rapidly, often with blanching, pain, and delayed capillary refill.

What Leads to Bruises vs. What Causes Vascular Occlusion?
Bruises are caused by trauma to the blood vessels beneath the skin. In aesthetic treatments, this typically happens when a needle punctures or grazes a small vessel during injection. Contributing factors include superficial injections, the use of sharp needles, and the patient's use of blood thinners.
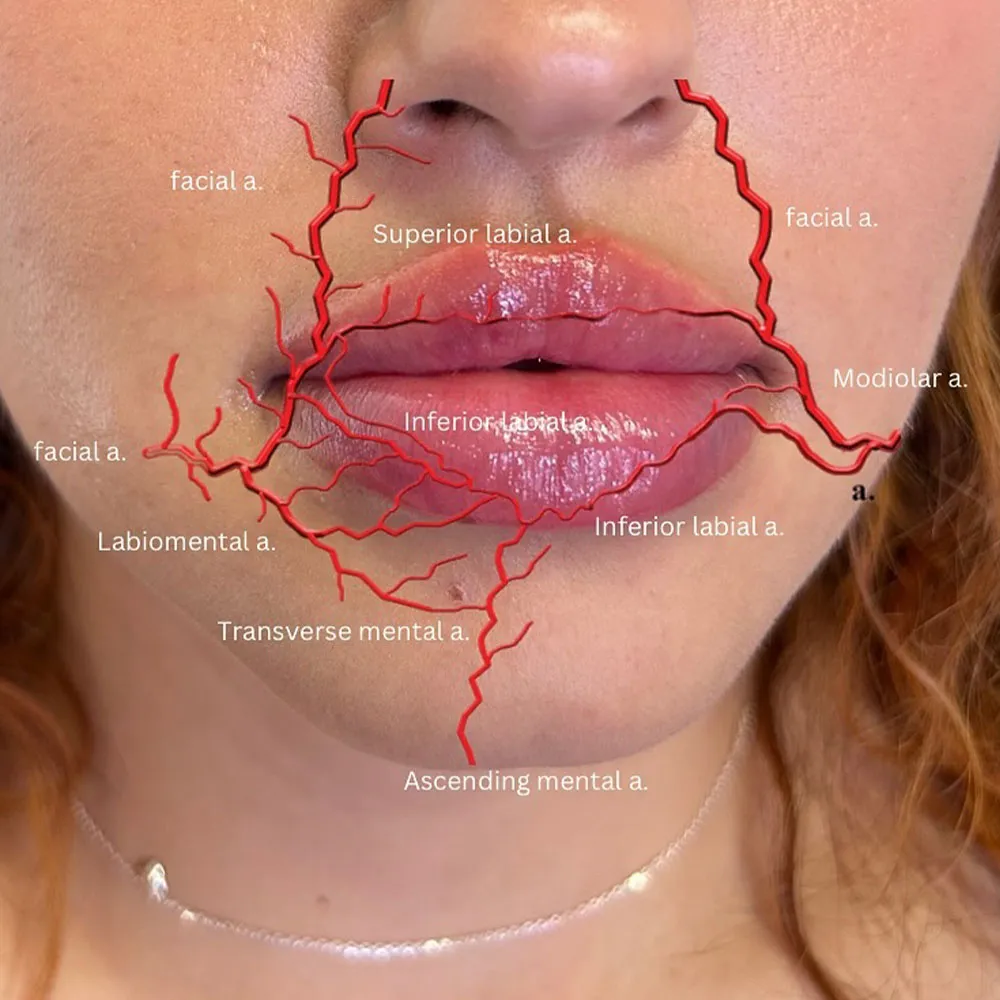
Vascular occlusion, conversely, results from filler entering and obstructing an artery or vein. This can happen due to poor injection technique, high pressure during injection, or injections too close to high-risk vascular areas. Lack of anatomical knowledge significantly increases the risk.
The key distinction lies in severity: bruising is temporary and cosmetic, while vascular occlusion is a medical emergency.
Identifying Whether It’s a Bruise or Vascular Occlusion
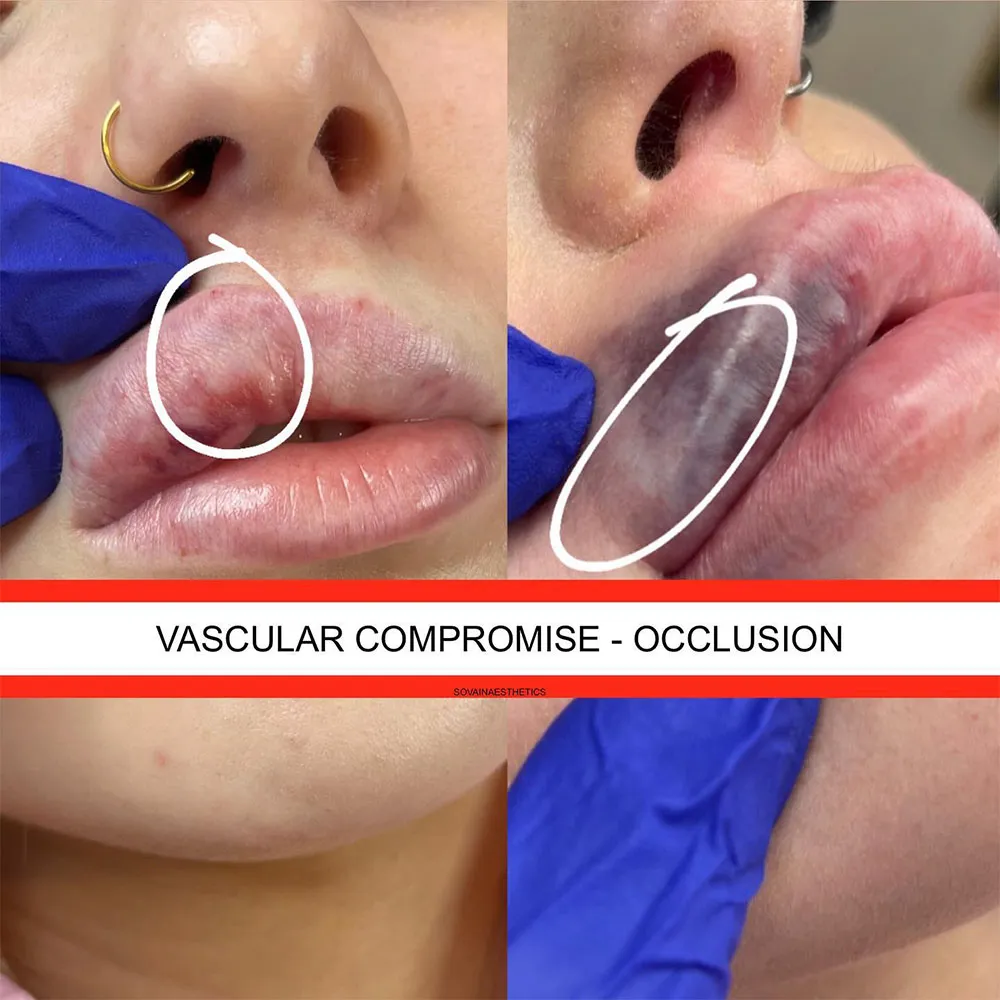
Correct identification relies on evaluating three main criteria: visual signs, timing, and pain. A bruise typically appears purple, blue, or green and may spread over time. Signs of vascular occlusion after filler often present with blanching, a reticulated (net-like) pattern, or dusky discoloration.
Timing also matters. A bruise may show up immediately or develop within a few hours and then fade. A vascular occlusion might have a delayed onset but will rapidly worsen if left untreated. Pain levels can also differentiate the two: bruises cause mild tenderness, whereas vascular occlusion causes sharp, escalating pain.
Professional education is key to mastering these distinctions. A certified aesthetics complications course offers essential training in identifying emergencies like vascular occlusion, while the Lip Augmentation Training masterclass provides the practical skills necessary for safe and effective filler procedures. These training programs help clinicians better interpret the early signs of both bruising and more serious complications.

Bruising or Vascular Occlusion: Cheek, Lip, and Chin Considerations
Location can help determine whether you’re observing a bruise or a vascular occlusion. In the cheek, bruises tend to be superficial and may not be accompanied by pain. A vascular occlusion in this area can cause blanching near the zygomatic arch or nasolabial fold and be accompanied by swelling and discomfort.
Lip filler bruising is common due to the high vascularity. However, if the patient experiences intense pain, purple or white discoloration, and firmness, it could be a vascular occlusion lip filler symptom.
In the chin area, bruises may present as swelling or mild discomfort. Vascular occlusion, however, typically causes firm, cool skin with reduced capillary refill. Understanding these regional differences enhances your diagnostic ability.
Risk Factors for Developing Vascular Occlusion or Bruise
Understanding what makes a patient more susceptible to bruising or vascular occlusion helps both in planning and managing treatments. For bruises, risk factors include patients with fragile or aging skin, those who smoke, or individuals on medications and supplements that thin the blood. Aggressive or repeated needle entry can also increase bruising risk.
Patients with prior facial surgery, vascular anomalies, or autoimmune conditions may also be at greater risk. Additional factors include poor hydration, high caffeine intake, recent alcohol consumption, and intense physical activity before or after treatment. Recognizing these factors during assessment and consultation allows for tailored risk management.
How to Prevent Bruises and Vascular Occlusion?
Preventing complications begins long before the first injection. To minimize bruising, educate patients on pre-treatment protocols such as avoiding alcohol, aspirin, and blood-thinning supplements. During the procedure, opt for blunt-tip cannulas when feasible and avoid excessive manipulation of the tissue. Gentle pressure and post-procedure cold compresses can further reduce bruising.
Preventing vascular occlusion requires careful technique and planning. Always aspirate before injecting and use slow, low-pressure delivery. Be particularly cautious in high-risk areas such as the glabella, nose, and lips. Choosing appropriate products, using smaller volumes, and maintaining awareness of facial anatomy are critical. Continued hands-on training and supervised practice sessions reinforce these safety measures.

Immediate Steps to Take in Case of Vascular Occlusion
If you suspect a vascular occlusion, act fast since every minute counts. The following protocol is recommended:
- Stop the injection immediately.
- Massage the affected area to help disperse the filler.
- Apply warm compresses to encourage blood flow.
- Administer hyaluronidase in high doses and repeat as necessary.
- Monitor the area and reassess every 30 minutes.
- Refer the patient to an emergency facility or vascular specialist if symptoms persist.
Having a vascular occlusion emergency kit ready and ensuring all staff are trained can save tissue and prevent long-term damage.
Why Knowing the Difference Is Critical for Patient Safety?
Knowing whether you are dealing with a bruise or a vascular occlusion is not just about clinical knowledge, it’s about protecting your patient’s well-being. Misdiagnosing a vascular occlusion as a bruise can result in disastrous consequences, including irreversible skin necrosis, disfigurement, or even blindness in severe cases. These risks highlight the importance of accurate, timely decision-making.
In contrast, mistaking a minor bruise for a more severe issue can cause undue anxiety for the patient and may lead to unnecessary treatments. Proper education and clinical judgment allow practitioners to respond appropriately without overreacting or underestimating symptoms.
Clinical Tips for Quick Assessment
Quick assessments are critical in determining whether a reaction is a benign bruise or a potentially dangerous vascular occlusion:
- Begin by visually inspecting the treatment area. Look for color changes such as purple, blue, or green hues indicative of a bruise, versus pale, white, or dusky discoloration that may signal vascular compromise. A reticulated or mottled pattern is particularly concerning.
- Evaluate the patient’s description of pain. Ask whether the discomfort is mild and dull which often indicates bruising, or sharp, intense, and worsening which could be a warning sign of vascular occlusion. Encourage honest feedback, even post-treatment.
- Tactile evaluation is another essential step. Use your fingers to gently press the skin and assess the temperature. Cool or firm areas are red flags. Perform a capillary refill test by pressing and releasing the skin. Anything longer than two seconds for color to return may suggest impaired circulation.
- Take clinical photographs immediately and at regular intervals to track progression. Documentation helps in decision-making and is valuable for medicolegal records.
- Educate your patients about red flag symptoms and empower them to contact your clinic immediately if issues arise, even after hours. Early reporting from the patient side is often the key to prompt intervention and successful outcomes.
The Bottom Line
Understanding whether you’re dealing with a bruise or vascular occlusion is a critical skill for any medical aesthetician. The ability to recognize the difference can prevent serious harm and ensure patient safety.
Invest in proper education and emergency preparedness, and familiarize yourself with signs, timelines, and protocols through professional courses. By mastering this knowledge, you protect your patients and also elevate the standard of care in aesthetic medicine.
References:
- King, M.; et al. Management of a Vascular Occlusion Associated with Cosmetic Injections. PMC - JCAD. 2020. https://pmc.ncbi.nlm.nih.gov/articles/PMC7028373/
- Schelke, L.; et al. Incidence of Vascular Obstruction After Filler Injections. PMC. 2020. https://pmc.ncbi.nlm.nih.gov/articles/PMC7357869/
- Hamman, M.S.; et al. Minimizing Bruising Following Fillers and Other Cosmetic Injectables. PMC – JCAD. 2013. https://pmc.ncbi.nlm.nih.gov/articles/PMC3760599/
- Martyn King. The Management of Bruising following Nonsurgical Cosmetic Treatment. PMC – JCAD. 2017. https://pmc.ncbi.nlm.nih.gov/articles/PMC5367875/
- Singh, K. and Nooreyezdan, S. Nonvascular Complications of Injectable Fillers—Prevention and Management. ResearchGate. 2020. https://www.researchgate.net/publication/347972442_Nonvascular_Complications_of_Injectable_Fillers-Prevention_and_Management
Disclaimer:
This article is intended for licensed medical professionals. All protocols, dosages, and treatment insights referenced herein are based on published literature. The content is not intended to encourage application, diagnosis, or self-treatment of unlicensed individuals, and should not be used as a substitute for the clinical judgment of a qualified healthcare provider.


