
The prejowl sulcus is a frequently overlooked yet critical feature of facial aging. As the region between the chin and jowl begins to hollow, it disrupts jawline continuity and creates a prematurely aged or tired appearance. Correctly diagnosing and treating this feature requires a deep understanding of lower facial anatomy, volume loss dynamics, and precise injection technique.
In-depth knowledge of prejowl sulcus treatment, dermal filler planning, and lower face rejuvenation strategies is essential for achieving harmonious jawline contour and natural outcomes. Refining injection technique and anatomical assessment through jawline filler training or enrolling in other HubMed Ed’s aesthetic courses for practitioners can enhance treatment outcomes and patient satisfaction.
Key Takeaways
- The prejowl sulcus is primarily a volume deficit, not just jowling.
- Comprehensive assessment ensures balanced outcomes.
- Filler choice, correct depth, and safety precautions are essential.
- Combined approaches often yield the most natural results.
What Is the Prejowl Sulcus?
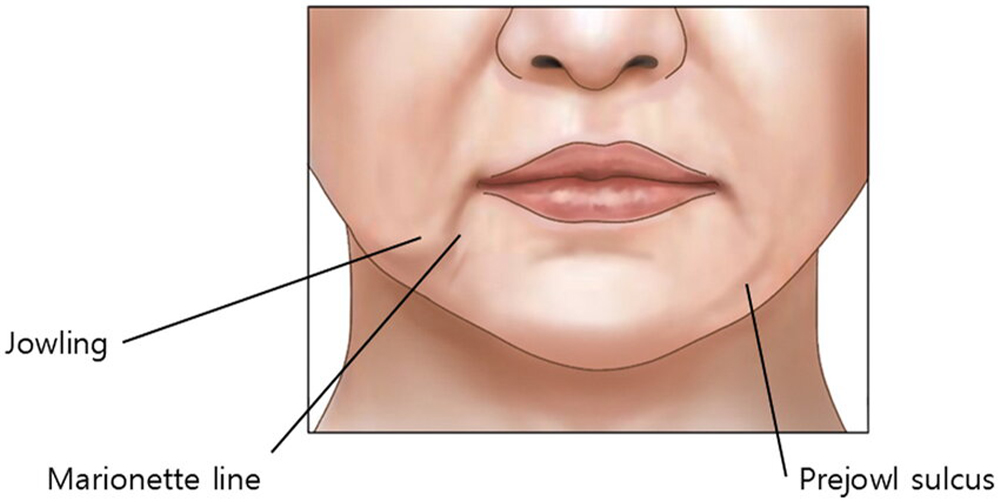
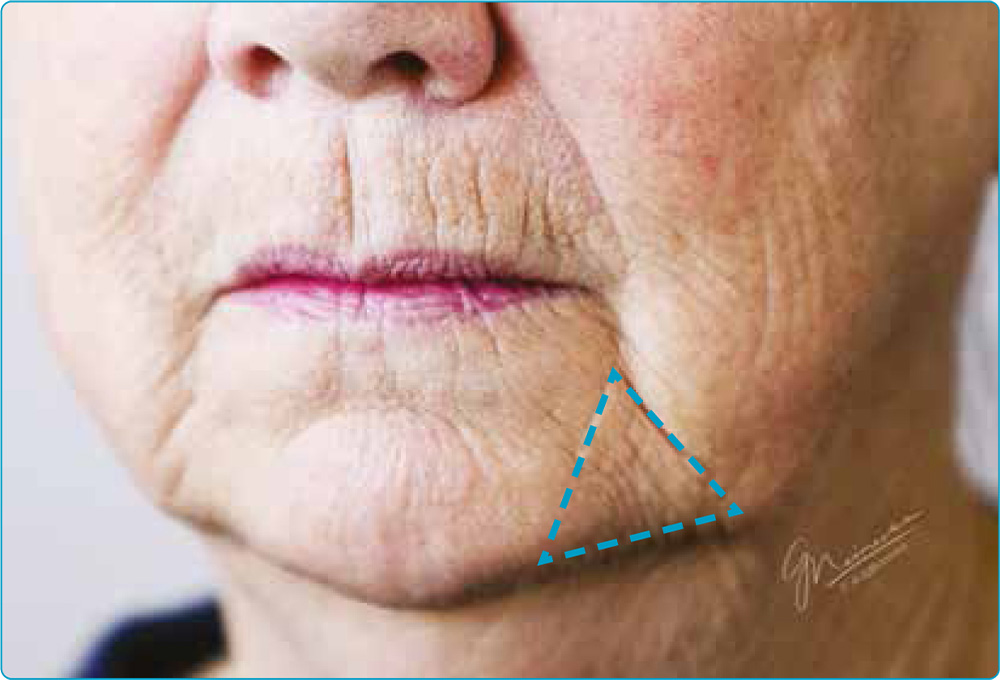
The prejowl sulcus is a linear hollow or depression that forms along the jawline, lateral to the chin, and medial to the jowl. Often misdiagnosed as early jowling, the sulcus itself represents a distinct anatomical volume deficit.
This groove disrupts the straight mandibular contour and contributes significantly to facial aging. It is especially apparent in female patients with thinner skin or significant soft tissue atrophy. Clinically, it is a critical landmark in lower facial rejuvenation planning, as its correction can drastically improve aesthetic balance.
Why Does the Prejowl Sulcus Form?
The prejowl sulcus results primarily from age-related changes, including bone resorption and soft tissue volume loss. The anterior mandible undergoes resorption with age, reducing skeletal support for overlying fat compartments and ligaments.
Additionally, the mandibular retaining ligament loses structural tension, allowing tissues to descend. When jowls begin to form, they accentuate the prejowl hollow even further. Genetics, UV exposure, smoking, and dramatic weight fluctuations can speed up these structural changes.
How Fat Removal Contributes to the Prejowl Sulcus?
Fat removal procedures such as buccal fat reduction and jowl liposuction have become popular, particularly due to celebrity influence and the desire for sharply contoured cheeks. However, removing too much fat from the lower face can unmask or worsen the prejowl sulcus, making it more noticeable when underlying fat support is reduced.
While fat removal does not directly cause the prejowl sulcus, it can reveal or deepen the hollow in individuals who are anatomically predisposed due to bone resorption, thin skin, or ligament laxity. Without sufficient volume, ligamentous tethering becomes more visible, and the jawline may lose continuity.
Patients with naturally low facial fat or early signs of volume loss are especially at risk. It is important to assess facial balance carefully before recommending fat-removal procedures and to consider combining them with dermal filler treatment to preserve or restore jawline harmony.

How to Assess Patients with Prejowl Sulcus
Accurate assessment of the prejowl sulcus is the foundation of successful aesthetic treatment. A detailed facial evaluation allows practitioners to distinguish between volume loss and structural descent, ensuring appropriate intervention:
- Examine overall jawline symmetry and identify areas of hollowing versus tissue descent.
- Use palpation to assess the depth and anchoring of the mandibular retaining ligament.
- Assess chin projection and prominence in profile view.
- Evaluate adjacent structures such as marionette lines and labiomental fold.
- Determine mandibular bone support and soft tissue coverage.
- Use standardized before-and-after photographs to document contour changes.
- Identify whether filler, skin tightening, or surgical referral is the most appropriate route based on severity.
Dermal Filler Treatment Strategies for the Prejowl Sulcus
Prejowl sulcus treatment with dermal fillers plays a central role in modern non-surgical jawline enhancement. It targets the key anatomical depression between the chin and jowl and restores structural continuity to the lower face.
Prejowl filler techniques continue to evolve, offering both immediate and long-term correction options depending on product choice and anatomical precision. The primary goal of treating the prejowl sulcus with dermal fillers is to restore a smooth, continuous jawline and camouflage the appearance of early jowling. Success depends on selecting the right product and technique tailored to the patient’s facial anatomy and degree of volume loss. High G’ fillers like Juvéderm Volux, Restylane Defyne, Radiesse, or Ellansé are typically preferred due to their structural support and lifting capacity.

Layering and Blending
In cases where the sulcus is shallow but sharply defined, layering a softer filler superficially can help smooth transitions between anatomical zones. This dual-plane strategy, deep structural support with high G’ filler and surface refinement with a low G’ filler, creates a more natural result. Avoid overcorrection, especially in female patients, where a bulky jawline can masculinize the face.
Product rheology plays an important role in this approach. Use high G’ fillers in the deep plane to restore mandibular contour and low G’ fillers superficially for dermal softening. Always blend transitions to avoid step-offs between treated and untreated zones. Use gentle massage post-injection, if appropriate, to improve integration and surface smoothness.
Dosage and Volume Considerations
Volume requirements vary by patient but typically range from 0.5 to 1.5 mL per side. Conservative dosing with staged treatment is advised to prevent overtreatment and allow for refinement. Combining prejowl filler with chin projection and marionette line correction often yields the most aesthetically pleasing results.
Factors such as gender, skin thickness, bone projection, and degree of soft tissue laxity should guide volume decisions. In patients with significant hollowness or strong mandibular anatomy, higher volumes or biostimulatory fillers may be appropriate. For subtle correction in younger patients, microbolus techniques or needle microdroplets may be preferred.
Always reassess after initial treatment before layering additional product. Encourage patients to return for follow-up after 2-4 weeks, when swelling subsides and contouring can be more accurately evaluated for symmetry and balance.
Safety Protocols in Prejowl Sulcus Filler Treatment
Ensuring patient safety in prejowl sulcus filler procedures requires anatomical precision, technique mastery, and best practices. Because this region lies near critical vascular structures, proper planning and technique are non-negotiable to minimize complications and maximize outcomes:
- Maintain depth control by injecting in the preperiosteal plane and avoiding superficial boluses that may cause lumpiness.
- Prioritize continuous education through VOD trainings and certified anatomical masterclasses focused on jawline contouring and lower face filler safety.
- Always use aspiration and slow injection techniques to minimize the risk of vascular compromise.
- Consider using a blunt-tip cannula to reduce the likelihood of arterial trauma in high-risk zones.
- Avoid overfilling, especially in female patients, to preserve natural jawline proportions and avoid masculinization.
- Inform patients of all potential adverse effects, including swelling, tenderness, asymmetry, and the rare risk of vascular events.

Adjunctive and Combined Approaches
Complementary treatments can enhance the results of prejowl sulcus filler procedures, especially in patients with tissue laxity or deeper structural aging. A combination of modalities often yields more natural and longer-lasting outcomes:
- Radiofrequency (RF) skin tightening: Helps improve skin elasticity and support along the jawline.
- Microfocused ultrasound (e.g., Ultherapy): Targets deeper dermal layers to stimulate collagen production and mild lifting.
- PDO threads: Provide mechanical lift and stimulate neocollagenesis; ideal for patients with mild jowling or poor skin tone.
- Biostimulatory fillers (e.g., Radiesse, Ellansé): Used in conjunction with HA fillers for long-term collagen support.
- Chin and marionette line correction: Enhances jawline continuity and lower face balance when treated alongside the prejowl sulcus.
- Surgical interventions: In advanced cases with severe tissue descent, lower facelift or prejowl implant surgery may be recommended.
- Maintenance protocols: HA fillers typically require re-treatment every 12-18 months, while biostimulants may offer extended results with fewer sessions.
Final Words
Whether you’re addressing mild contour irregularities or performing full jawline rejuvenation fillers, success depends on correct diagnosis, technique, and patient selection.
The prejowl sulcus is a hallmark of lower face aging that subtly yet significantly disrupts aesthetic harmony. Dermal fillers, when selected appropriately and placed with anatomical precision, offer a non-surgical solution to restore jawline smoothness and facial proportion.
Aesthetic professionals seeking to enhance their results should invest in expert VOD aesthetic courses and masterclasses at HubMed Ed covering lower face anatomy, prejowl filler techniques, and safe injection protocols.
FAQs
What is the best filler for pre-jowl sulcus?
Juvéderm for jowls is the most popular dermal filler for this area of the face, with Restylane and Radiesse close behind. However, the choice of filler depends on individual anatomy and clinical judgment, as medical assessment will determine which product offers the best structural support and aesthetic result for each patient.
How long does pre-jowl filler last?
Longevity varies by product, but most HA fillers last 12-18 months. Biostimulatory fillers may last longer with collagen remodeling.
What is a prejowl implant?
A prejowl implant is a surgical silicone or solid implant placed lateral to the chin to fill the hollow and correct jawline depression.
Who is not a candidate for jaw fillers?
Patients with active infections, autoimmune disorders, or unrealistic expectations should not undergo filler treatments.
Can I get rid of jowls without surgery?
Mild to moderate jowling can be improved with fillers, RF, ultrasound, or threads. Severe jowling may require surgical intervention.
Where do you put fillers for sagging jowls?
Fillers are placed in the prejowl sulcus, chin, and lateral jawline to restore contour and provide lift, depending on the degree of sagging.
References:
- Talei B, Ziai H. Mandibular Ligament and the Prejowl Sulcus Explained. Aesthet Surg J. 2024 Oct 15;44(11):1131-1139. doi:10.1093/asj/sjae151. https://pubmed.ncbi.nlm.nih.gov/39001648/
- Braz A, Eduardo CC de P. Reshaping the Lower Face Using Injectable Fillers. Indian J Plast Surg. 2020 Aug;53(2):207–218. doi:10.1055/s-0040-1716185. https://pmc.ncbi.nlm.nih.gov/articles/PMC7458843/
- Jewell T. Jowls: Why It Happens and What You Can Do. Healthline. Updated November 16, 2023. Accessed August 27, 2025. https://www.healthline.com/health/beauty-skin-care/jowls
Disclaimer:
This article is intended for licensed medical professionals. All protocols, dosages, and treatment insights referenced herein are based on published literature. The content is not intended to encourage application, diagnosis, or self-treatment of unlicensed individuals, and should not be used as a substitute for the clinical judgment of a qualified healthcare provider.

