
Key Takeaways
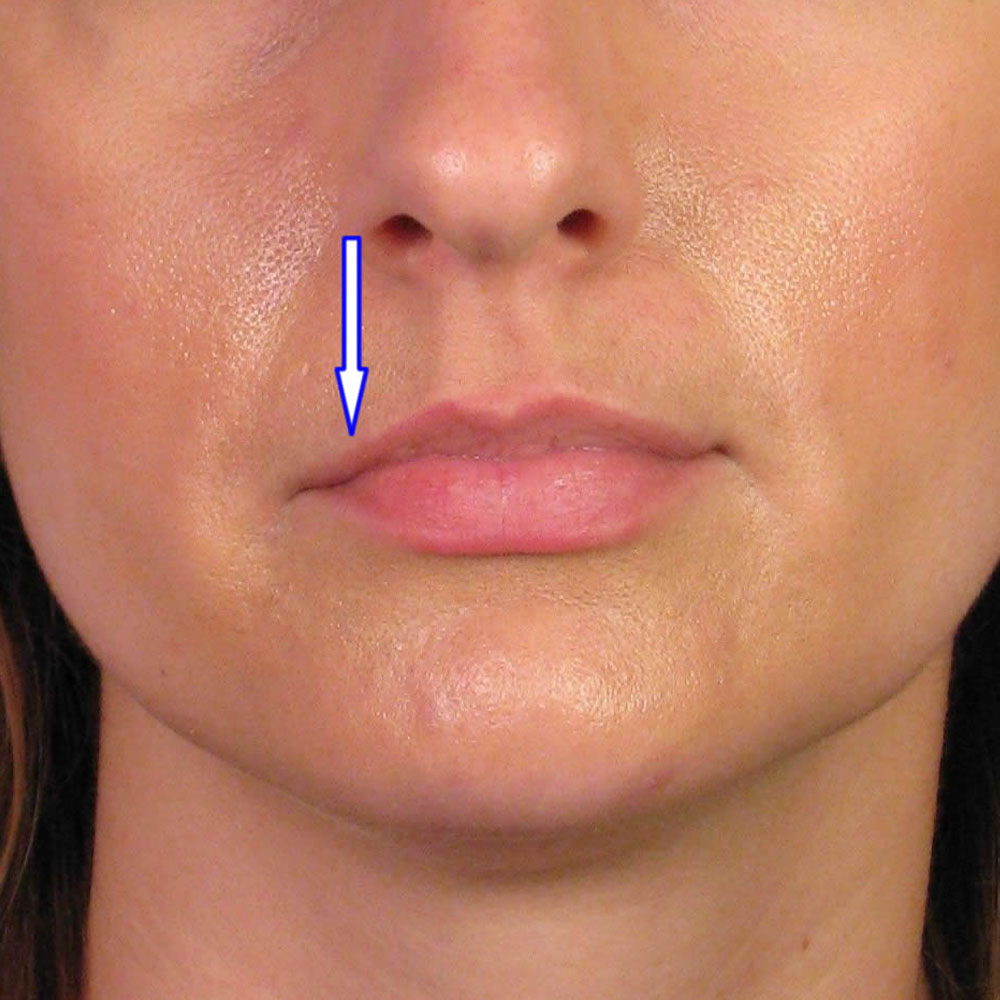
- Lip ptosis refers to drooping of the upper or lower lip, which can be temporary (after Botox) or structural (due to aging or anatomy).
- Common lip ptosis causes include Botox diffusion, muscle weakness, natural aging, and structural imbalances.
- Lip ptosis correction strategies may involve Botox adjustments, dermal fillers for lip droop, or surgical intervention in severe cases.
- Patient education is crucial: realistic expectations, understanding treatment limits, and proper aftercare can improve results.
- Not everyone is a good candidate for lip ptosis treatment; correct diagnosis and injector expertise are essential.
Have you ever had a patient come in worried that their smile looks uneven or that their lip seems to droop more than usual? This is often what we call lip ptosis, or “drooping lip,” and it can be just as frustrating for patients as it is for practitioners trying to correct it. While sometimes temporary, like when Botox spreads into the wrong muscle, it can also be a long-term concern linked to aging or anatomy. For medical aestheticians, knowing the difference is key. In this guide, we’ll break down the most common lip ptosis causes, explore correction strategies with Botox and dermal fillers, and cover the essentials of patient education and safe practice.
What Is Lip Ptosis?
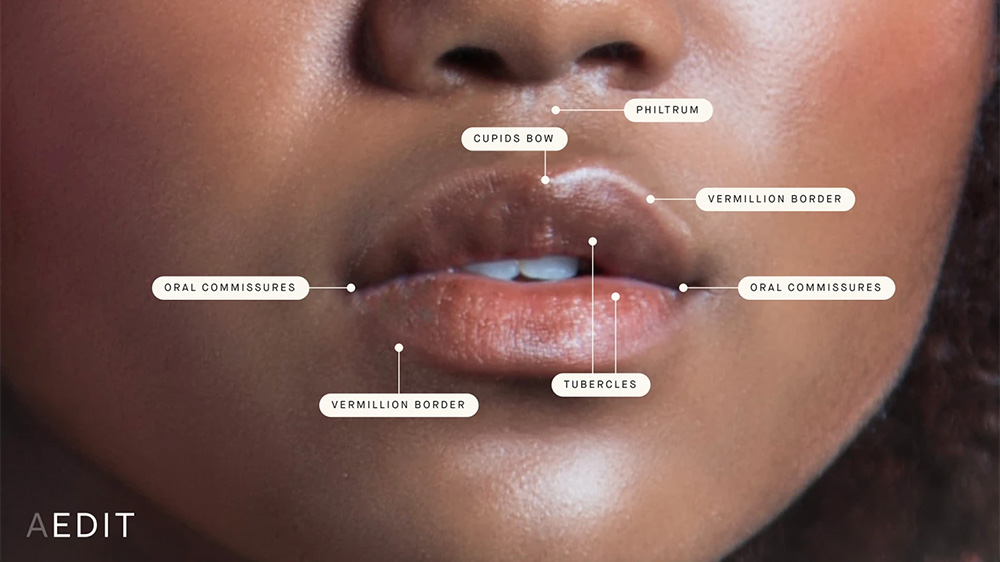
Lip ptosis refers to the downward drooping of the upper or lower lip. It may occur after injectable treatments like Botox, or it may develop naturally over time due to aging and muscle changes. Patients often seek lip ptosis treatment because drooping lips can impact facial balance, speech, or even oral function. For many, the motivation is both cosmetic and functional, wanting to restore symmetry and confidence.
There are two main types:
- Temporary lip ptosis: Often linked to injectable treatments such as Botox diffusing into surrounding muscles.
- Structural lip ptosis: Caused by natural aging, loss of muscle tone, or congenital conditions.
Lip Ptosis Causes
Several factors contribute to lip ptosis:
- Botox diffusion: One of the most common lip ptosis causes occurs when Botox spreads beyond the intended injection site, weakening muscles that support the lips. This is often seen in lip ptosis after Botox.
- Aging process: Over time, the orbicularis oris muscle weakens, and collagen loss reduces skin elasticity, leading to lower lip ptosis or upper lip ptosis.
- Anatomical variations: Some individuals naturally have weaker muscle support or asymmetry that predisposes them to lip droop ptosis.
- Surgical or trauma-related changes: Procedures involving the mouth or scarring may cause drooping lips.
- Filler-related issues: While less common, lip ptosis after filler may occur if product placement affects muscle movement.
Lip Ptosis Correction Strategies
Correction requires a tailored approach based on whether the ptosis is temporary or structural.
- Botox lip ptosis correction: If ptosis develops after Botox, time is often the best solution as the product naturally wears off. In some cases, small adjustments with targeted injections can help balance movement.
- Dermal fillers for lip droop: Fillers can restore volume and support around the lips, helping correct sagging. Proper lip ptosis injection strategy ensures natural results while avoiding additional droop.
- Lip ptosis surgery: In severe or structural cases, surgical lifting may be necessary to reposition the lip.
- Supportive therapies: Some patients explore lip ptosis exercises to stimulate muscle tone, though these have limited evidence compared to injectables.
Key Information Before Lip Ptosis Treatment
Patient education is essential for successful outcomes. Aestheticians should clarify:
- Temporary vs. structural ptosis: Explain whether the droop is caused by Botox, aging, or anatomy.
- Treatment timeline: Correction may take multiple sessions, especially with dermal fillers for lip droop.
- Injector expertise: Lip ptosis correction requires strong anatomical knowledge and precise injection skills. Training such as lip enhancement training can help practitioners gain confidence in these techniques.
- Expectations: While improvement is achievable, complete reversal may not be possible in all cases.
What Not to Do During Lip Ptosis Correction
When working with lip ptosis, small mistakes can make the condition worse instead of better. A few things are important to keep in mind. For injectors, avoid placing Botox too close to the orbicularis oris muscle, as even a slight spread can weaken the wrong area and create more drooping. Overfilling with dermal fillers is another common issue; it may distort movement and add heaviness rather than support. From the patient's side, simple habits like pressing, massaging, or applying heat to the treated area can interfere with healing and product placement. Finally, practitioners should never attempt these corrections without specific training, since managing complications requires experience. For those seeking to refine their skills, the advanced programs like the aesthetic complications course provide useful guidance for managing risks.
Who Is Not a Good Candidate for Lip Ptosis Treatment?
Not all patients are suitable for lip ptosis correction. Those with severe muscular or neurological conditions may not respond well to injectables. Additionally, patients with unrealistic expectations or who seek immediate results may be poor candidates. Careful assessment and patient selection are crucial.
Patient Education and Expectation Management
With lip ptosis, what patients understand about the process can make or break the outcome. It’s important to be clear about whether their droop is likely temporary, such as lip ptosis after Botox, or structural, which may require a longer-term approach. Patients also need to know that results don’t always happen overnight; in many cases, it can take a few sessions to achieve the desired balance.
Conversations around expectations should always be realistic. Complete correction isn’t possible for everyone, but noticeable improvement often is. This is where trust in the injector’s expertise matters most. Patients should feel confident that their provider understands facial anatomy and can create a plan tailored to their needs.
Aftercare guidance is another part of education that shouldn’t be overlooked. Simple advice, like avoiding pressure, massage, or heat near the lips in the hours after injections, can make a big difference in recovery and results. In short, honest communication and practical instructions help patients feel supported while ensuring their treatment has the best chance of success.
For aestheticians looking to strengthen their expertise, exploring HubMed Ed’s popular online aesthetic courses for doctors can provide additional learning opportunities.

FAQ: Lip Ptosis
At what age does ptosis start?
Ptosis can develop at any age, but is more common with aging due to muscle weakening. Most patients notice lip droop in their 40s or 50s, though earlier onset is possible.
How to reverse droopy lips?
Options include Botox adjustments, dermal fillers, or surgery in advanced cases.
Can ptosis go away by itself?
Temporary lip ptosis after Botox usually resolves as the product wears off.
Does insurance cover ptosis surgery?
Functional cases may qualify, but cosmetic surgery is typically not covered.
Can Botox fix ptosis?
Patients should be careful, as Botox can actually worsen ptosis if incorrectly placed, but careful injections can sometimes help balance appearance.
Conclusion: How to Fix Lip Ptosis?
At the end of the day, fixing lip ptosis comes down to understanding its cause and choosing the right approach. If it’s temporary after Botox, patience is often all that’s needed. For age-related or structural drooping, dermal fillers or, in some cases, surgery can make a noticeable difference.
What matters most is clear communication with patients, setting realistic expectations, and relying on skilled injection techniques. With the right strategy, medical aestheticians can help patients feel more comfortable with their smile and restore confidence in a way that looks natural and balanced.
Sources:
- Motamedi MHK. Treatment of post-traumatic lower lip ptosis: report of case. J Oral Maxillofac Surg. 1996;54(2):230-233. doi:10.1016/s0278-2391(96)90748-2 https://www.joms.org/article/S0278-2391(96)90456-5/abstract
- Weston GW, Poindexter BD, Sigal RK, Austin HW. Lifting lips: 28 years of experience using the direct excision approach to rejuvenating the aging mouth. Aesthet Surg J. 2009;29(2):83-86. doi:10.1016/j.asj.2009.01.013 https://pubmed.ncbi.nlm.nih.gov/19371836/
- Austin HW, Weston GW. Rejuvenation of the aging mouth. Clin Plast Surg. 1992;19(2):511-524. https://pubmed.ncbi.nlm.nih.gov/1576793/
- Santanchè P, Bonarrigo C. Lifting of the upper lip: personal technique. Plast Reconstr Surg. 2004;113(6):1828-1837. doi:10.1097/01.prs.0000117661.07141.70 https://pubmed.ncbi.nlm.nih.gov/15114153/
Disclaimer:
This article is intended for licensed medical professionals. All protocols, dosages, and treatment insights referenced herein are based on published literature. The content is not intended to encourage application, diagnosis, or self-treatment of unlicensed individuals, and should not be used as a substitute for the clinical judgment of a qualified healthcare provider.

