
Key Takeaways
- Essential safety tool: Hyaluronidase is indispensable for both correcting poor outcomes and managing urgent complications like vascular occlusion.
- Protocol-driven use: Elective touch-ups require conservative dosing, while emergencies call for higher, repeated administrations guided by established guidelines.
- Patient demand is rising: More patients are requesting filler dissolution, especially for migrated or overfilled lip fillers, making injector expertise critical.
- Short-term effects: Swelling, redness, and tenderness are common after treatment, but visible improvement typically appears within 24–48 hours.
- Training is key: Proficiency in anatomy, dosing, and complication management should is imperative, so professionals should focus on extensive training in aesthetics complications management for injector safety and patient trust.
What Is Hyaluronidase?
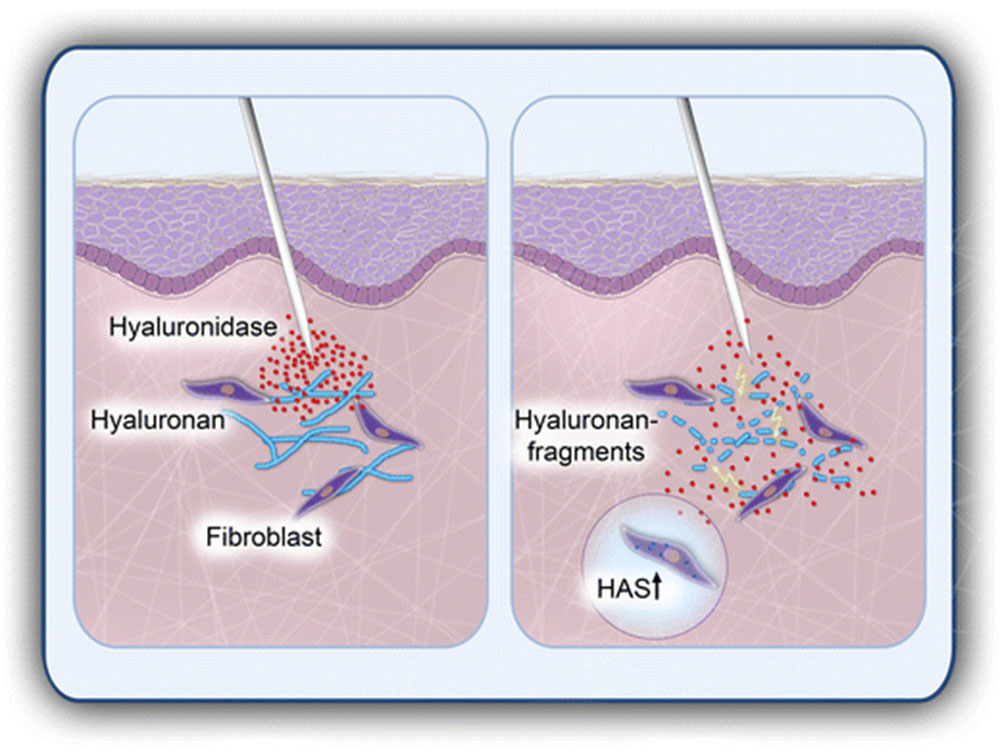
Hyaluronic acid is a naturally occurring substance found in connective tissue and the main component in most dermal fillers, and hyaluronidase is an enzyme that breaks it down. In aesthetic practice, it allows injectors to adjust or reverse results by dissolving unwanted filler or managing complications.
Unlike hyaluronic acid, which provides structure and hydration, hyaluronidase works by catalyzing the hydrolysis of hyaluronic acid chains, making them more easily absorbed by the body. This action makes it indispensable in both emergency and elective situations.

What Is Hyaluronidase Used For?
In clinical aesthetics, hyaluronidase has several applications:
- Correction of poor results: Patients may request to dissolve lip filler or temple filler when outcomes look unnatural.
- Emergency protocols: In cases of hyaluronidase vascular occlusion, rapid injection can restore blood flow and prevent tissue necrosis.
- Overcorrection or migration: Hyaluronidase is used when filler moves outside the target zone, such as filler migration in lips.
- Diagnostic tool: Small test doses may be used to confirm a suspected filler-related nodule.
Its dual role as both a corrective and emergency agent makes it one of the most important safety tools in modern aesthetic practice.
How Is Hyaluronidase Used in Aesthetic Medicine?
Administration requires a detailed understanding of facial anatomy. Hyaluronidase is typically reconstituted with saline and injected directly into the area where filler is located. The dosage depends on the volume of filler present and whether treatment is elective or emergent.
- Elective correction: Lower doses, carefully titrated over one or more sessions.
- Emergency use (vascular occlusion): Higher, repeated doses, guided by established hyaluronidase protocols aesthetics guidelines such as those from the ACE Group.
Practitioners are advised to carry hyaluronidase in every clinical setting where dermal fillers are performed, as it can mean the difference between full recovery and permanent damage in vascular emergencies.
Why Are Patients Choosing to Dissolve Fillers?
Patients seek hyaluronidase treatment for several reasons. A common motivation is dissatisfaction with the aesthetic outcome, such as asymmetry or overfilled lips. Others choose it after experiencing filler migration, particularly in sensitive areas like the lips or under-eyes.
In some cases, patients want to return to their natural appearance or reset their baseline before trying a different filler technique. As demand for hyaluronidase for lip filler grows, injectors must balance patient expectations with safety protocols.
Does Hyaluronidase Completely Dissolve Fillers?
Yes, hyaluronidase can fully break down hyaluronic acid fillers, though the extent depends on dosage and injection technique. In some cases, small amounts of filler may remain, especially if the product was highly cross-linked. Patients requesting complete removal often require follow-up treatments to achieve full resolution.

Hyaluronidase Administration and Patient Experience
Administering hyaluronidase requires careful preparation and a clear treatment plan. The enzyme is typically supplied as a powder and reconstituted with saline before use. Dosage depends on the indication: in elective cases, such as refining overfilled lips or correcting asymmetry, a conservative approach is taken, often with staged sessions. In emergencies like hyaluronidase vascular occlusion, higher doses are delivered promptly, sometimes in repeated administrations, to restore perfusion and minimize the risk of tissue loss.
The choice of injection technique varies by area and clinical goal. A fine needle or blunt cannula may be used, with many practitioners favoring cannulas for added safety in high-risk zones. Injectors should aspirate where appropriate, inject slowly, and monitor patient comfort throughout the procedure.
What to expect after hyaluronidase treatment:
From the patient’s perspective, treatment is generally quick but may involve mild discomfort. A brief stinging or burning sensation is common as the enzyme is introduced. Redness, swelling, and tenderness at the injection site often appear immediately after but usually resolve within a few days. Visible improvement from using hyaluronidase for dissolving filler is often noted within 24 to 48 hours, though full assessment is best made after one week, once swelling subsides and tissue balance is restored.
Setting clear expectations is key. Patients should be informed that hyaluronidase acts on all hyaluronic acid present in the treated area, meaning it may also break down some of their body’s natural stores of hyaluronic acid. Reassurance is important, as the body replenishes its own supply over time. A thorough discussion before treatment helps patients understand both the benefits and the limitations of the procedure, strengthening trust and satisfaction.

How Long Does Hyaluronidase Last?
Hyaluronidase works rapidly but remains active in tissue for about 24–48 hours. During this time, it continues to degrade hyaluronic acid until it is neutralized by the body. This is why results may keep evolving for several days post-treatment.
For elective corrections, injectors often review the patient after one week to assess whether additional treatment is needed.
Hyaluronidase Side Effects and Risks
While generally safe, hyaluronidase does carry risks. The most common are temporary swelling, bruising, and mild discomfort. Less common but important considerations include:
- Allergic reactions: Though rare, hypersensitivity can occur. A patch test may be performed if risk is suspected.
- Overcorrection: In some cases, hyaluronidase may break down more filler than intended.
- Irregular texture: Especially if large volumes of filler are dissolved at once.
More information on hyaluronidase side effects can be found in our dedicated guide.
What Not to Do After Hyaluronidase
Patients should avoid massaging the treated area, as this may spread the enzyme beyond the intended zone. Strenuous exercise, heat exposure, and alcohol should also be avoided for at least 24 hours to reduce swelling and bruising.
How Long Does Filler Take to Dissolve with Hyaluronidase?
In most cases, filler breakdown is visible within 24–48 hours, though complete resolution may take up to a week. Highly cross-linked fillers may require multiple treatments.

Conclusion
Hyaluronidase is one of the most important safety tools in modern aesthetic medicine. It allows practitioners to correct results, manage emergencies, and maintain patient trust. Mastery of hyaluronidase protocols aesthetics, understanding of anatomy, and effective communication with patients are crucial for safe and predictable outcomes.
For those looking to refine their skills, explore our aesthetic medical training for doctors and advanced aesthetics complications training modules, covering vascular occlusion management and filler artistry.
FAQ
How long does lip filler take to dissolve with hyaluronidase?
Most lip fillers dissolve within 24–48 hours, though additional sessions may be needed for complete resolution.
Is hyaluronidase the same as hyaluronic acid?
No. Hyaluronic acid is the filler material, while hyaluronidase is the enzyme used to break it down.
Does hyaluronidase remove all fillers?
It only works on hyaluronic acid-based fillers, not on permanent or non-HA fillers.
Can you feel hyaluronidase working?
Some patients feel mild tingling or warmth as the enzyme begins to break down the filler.
How long will I be swollen after hyaluronidase?
Swelling usually lasts 24–72 hours and subsides as the tissue settles.
Sources
- Kim MS, Youn S, Na CH, Shin BS. Allergic reaction to hyaluronidase use after hyaluronic acid filler injection. J Cosmet Laser Ther. 2015;17(5):283-285. doi:10.3109/14764172.2015.1007069 Available from: https://pubmed.ncbi.nlm.nih.gov/25588036/
- ACE Group. Guidelines for the Use of Hyaluronidase in Aesthetic Practice. 2024. Available from: https://uk.acegroup.online/wp-content/uploads/2024/01/ACE-Group-Hyaluronidase-v3.1.pdf
- Urdiales-Gálvez F, et al. The Use of Hyaluronidase in Aesthetic Practice: A Comparative Study of Practitioner Usage in Elective and Emergency Situations. Aesthet Surg J. 2024;44(6):647–659. Available from: https://academic.oup.com/asj/article/44/6/647/7585836
- Murray G, Convery C, Walker L, Davies E. Guideline for the Safe Use of Hyaluronidase in Aesthetic Medicine, Including Modified High-dose Protocol. J Clin Aesthet Dermatol. 2021;14(8):E69-E75. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8570661/
Disclaimer:
This article is intended for licensed medical professionals. All protocols, dosages, and treatment insights referenced herein are based on published literature. The content is not intended to encourage application, diagnosis, or self-treatment of unlicensed individuals, and should not be used as a substitute for the clinical judgment of a qualified healthcare provider.

